Navigating the Ethical Landscape of Dialysis: Empowering Patient Advocacy and Rights
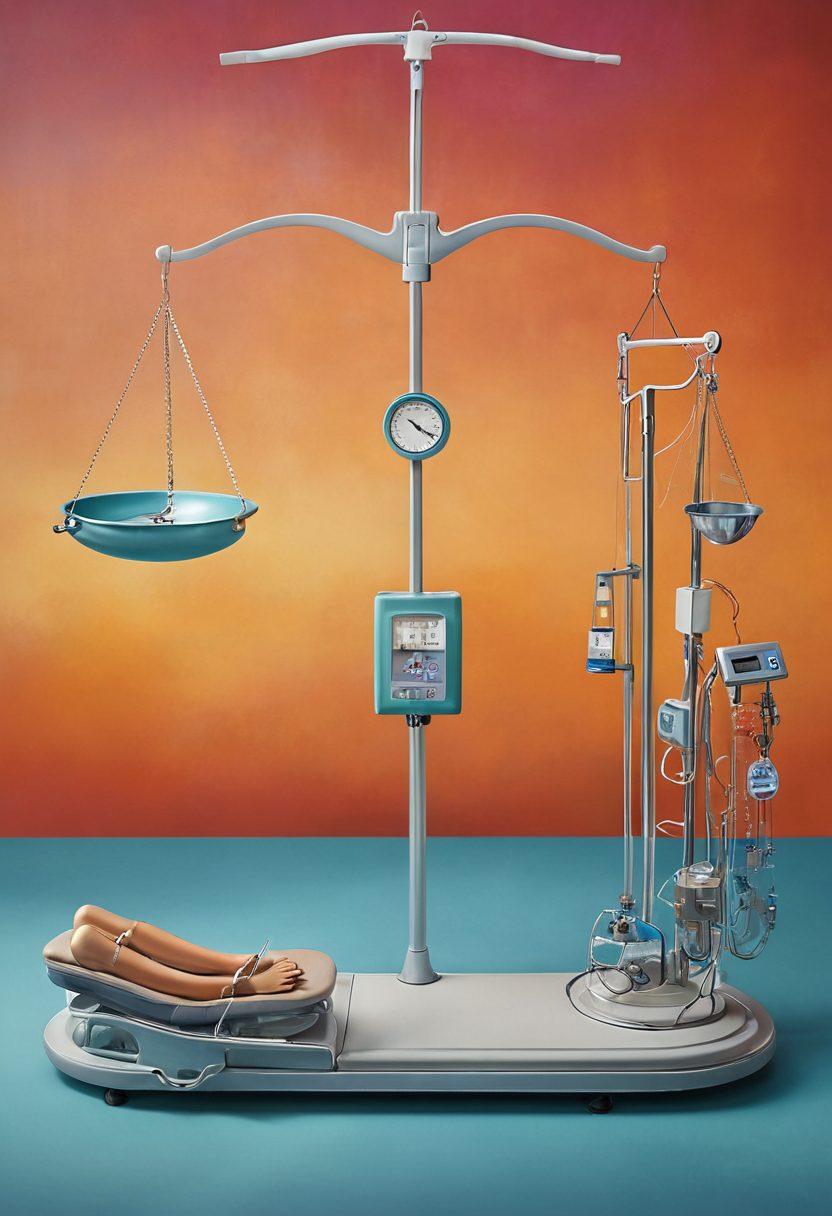
Imagine being faced with a chronic illness like chronic kidney disease, suddenly thrust into a world where every decision about your health feels daunting and overwhelming. The choices you make regarding dialysis treatment could be life-altering. Underpinning these choices is a crucial foundation: patient rights in dialysis. Understanding these rights is not only empowering but essential for anyone navigating the intricate waters of ethical dialysis care. In this blog, we will explore the intricate tapestry of patient rights, the ethical considerations in dialysis, and how these pivotal factors shape the delivery of quality care for patients.
At the heart of ethical dialysis is an emphasis on patient advocacy. When patients are informed about their rights, they become empowered participants in their healthcare decisions. This empowerment is not just a buzzword; it’s a fundamental aspect of healthcare ethics that demands informed consent in dialysis decisions. Are you aware of what your rights as a patient entail? Knowledge is power! For instance, patients have the right to understand their treatment options fully, to refuse any treatments they are uncomfortable with, and to seek second opinions when necessary. These rights should be viewed as cornerstones of ethical dialysis that guide every interaction between the patient and healthcare professionals.
Healthcare access plays a significant role in achieving equitable healthcare in dialysis. Most people do not realize the disparities that exist in dialysis care based on geographical and economic factors. The question remains: Why does access to high-quality dialysis care remain a challenge for so many? Patients often find themselves grappling with ethical dilemmas in dialysis, faced with the harsh reality that quality care is sometimes dictated by the resources available or the policies in place. Advocacy for patient rights and equitable healthcare in dialysis is essential to bridge these gaps and ensure everyone receives the treatment they so rightfully deserve.
As we dive deeper, let's not forget the ethics surrounding medical advancements in dialysis. Every innovation brings a complex layer of ethical governance and considerations. For instance, new dialysis methods or technologies enhance quality of care, but they also require patients to navigate a plethora of information. How do we balance innovation with comprehending what’s right for the individual patient? It’s crucial for healthcare providers to maintain a transparent dialogue with their patients, discussing not just what is available but also its implications, which ties back into informed consent in dialysis.
Ultimately, as we discuss the nuances of dialysis care and the ethical responsibilities that come with it, it is clear that patient protection in dialysis is paramount. A robust dialysis policy that prioritizes patient rights fosters a culture of respect, dignity, and individual choice. So, the next time you encounter someone battling chronic kidney disease or are faced with decisions related to dialysis treatment, remember: patient rights should always guide the ethical landscape of care. Together, through advocacy and informed choices, we can build a more equitable system for all.
Balancing Ethics and Access: Navigating the Complexities of Dialysis Treatment
Navigating the complex landscape of dialysis treatment can feel like a journey through uncharted waters. With the urgency of chronic kidney disease looming over patients and their families, the importance of understanding the ethical considerations in dialysis cannot be overstated. As we explore the delicate balance between ethics and access in dialysis treatment, we must initiate conversations around patient rights in dialysis and patient advocacy, ensuring that everyone can achieve the quality of care they deserve. More than just a medical procedure, dialysis engenders a critical discussion about healthcare access and ethical dilemmas that demand our attention.
Imagine, for a moment, being faced with a life-threatening health issue, relying on lifesaving treatments, yet feeling powerless to affect the decisions that govern your care. This is the stark reality for many who undergo dialysis. Patient protection in dialysis is not just a catchphrase; it is a fundamental right that should permeate every level of dialysis governance. Ethical dialysis practices should prioritize the needs and voices of patients, allowing them to navigate their treatment options with dignity and informed consent in dialysis. How can we ensure that patient-centered dialysis becomes a standard, rather than an exception?
As we delve deeper into the heart of kidney care ethics and the ethical dilemmas in dialysis, we uncover the intricate web of dialysis policy that shapes not only the availability of treatment but also its accessibility and efficacy. For patients grappling with chronic illnesses, equitable healthcare in dialysis is more than a benign ideal; it's a lifeline that determines their quality of life. The journey towards accessible dialysis treatment must include clear frameworks that elevate dialysis standards, demand transparency, and uphold the principles of healthcare ethics in the face of potential compromise. What steps can we collectively take to advocate for more ethical dialysis policies?
The emotional toll of chronic kidney disease is profound, often overshadowed by the physical challenges associated with dialysis care. Patients are not merely passive recipients of treatment; they are individuals with aspirations, fears, and rights. By emphasizing patient advocacy, we can push for crucial changes to the existing dialysis frameworks, ensuring that the voices of those affected resonate during policy-making processes. As agents of change, how can we collaborate with healthcare providers to create a culture surrounding renal care ethics where patients feel heard and valued?
When discussing the future of dialysis, one of the most pressing questions looms: how do we solidify ethical foundations while ensuring that all patients have access to necessary treatments? The fusion of bioethics in dialysis and patient-centered care practices can lead to transformative outcomes for individuals battling chronic kidney disease. By fostering a community of awareness and action regarding dialysis quality of care, we can develop a robust support system where patients know their rights and can actively engage in their treatment journeys. Are we ready to take on the challenge of reimagining dialysis access for the betterment of all?
Empowering Voices: Patient Advocacy in the Ethical Landscape of Dialysis
In the realm of healthcare, few topics stir the soul and spark vigorous debate quite like the ethical considerations surrounding dialysis. As a lifeline for those grappling with chronic kidney disease, dialysis offers hope but also brings forth a multitude of ethical dilemmas. How do we ensure patient rights in dialysis are prioritized? Can we navigate the intricate maze of dialysis ethics while uplifting patient advocacy? It’s essential to delve deeper into these questions, to understand the paramount importance of empowering patient voices in the ethical landscape of dialysis.
The journey through dialysis treatment can often feel overwhelming. Imagine sitting in a clinic, surrounded by buzzing machinery and the sterile smell of antiseptics, waiting for a session that could prolong your life. In that moment, how can we ensure that decisions about your care are not merely dictated by medical norms but are built around your personal wishes? Ethical dialysis must embrace patient-centered principles, recognizing the rights and perspectives of those who experience it firsthand.
Patient advocacy isn't just a buzzword; it's a fundamental pillar of ethical healthcare practices. Advocates for patient rights in dialysis aim to create an environment where patients feel their voices are heard and respected. Think of it as a canvas—each patient's unique story adds color and depth to the collective experience of renal care ethics. When patients share their stories, they not only highlight the nuances of their own experiences but also illuminate the need for equitable healthcare in dialysis for everyone.
An essential component of understanding dialysis policy and its implications is informed consent in dialysis. This process ensures patients make educated decisions about their treatment options, fostering a sense of empowerment that every individual deserves. Yet, what happens when patients feel overwhelmed or uninformed? Ethical considerations in dialysis require us to create systems that advocate for transparency and education, transforming what could be a chaotic experience into one of understanding and empowerment. Can you remember a time when you felt your choices were disregarded in a healthcare setting?
Finally, as we explore dialysis quality of care, we must not overlook the importance of continuous dialogue between patients, healthcare providers, and policymakers. Implementing strong dialysis protocols is vital, but equally important is ensuring that those standards are infused with patient ideals. What if every session of dialysis could become a space of shared advocacy? As advocates for healthcare ethics, we have the duty to champion patient protection in dialysis, ensuring that every voice counts, and that every patient's rights are safeguarded. The future of healthcare, especially in the realm of dialysis, is not just about treatment; it's about respect, empathy, and understanding in the art of healing.